How Real is Patient Centricity in Healthcare Today?
Updated: Oct 8, 2018
It is interesting (and ironic) that we have been enamored by the concept that patient care should place the patient at the center of it all. This in itself is telling – our healthcare systems are so complex that oftentimes, the patient is overlooked.
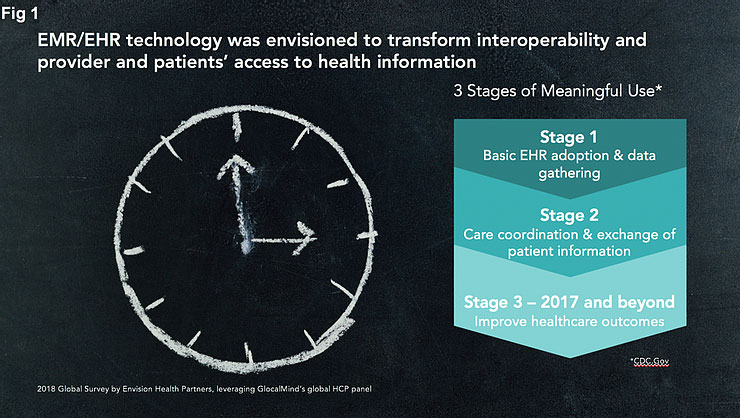
EHR/EMR systems were touted as one of the great technological innovations of the last decade. The vision was a data driven approach to achieving better health outcomes. Imagine if all patient data were digitized and stored on a platform? Imagine if patients and providers could access and share this information easily with other physicians and enable more comprehensive care and faster care?
The US healthcare industry has spent the better part of the last decade entering patient information into Electronic Medical Records in an attempt to realize (and frankly comply with) the great vision of a fully transparent, interconnected, interoperable system of patient information, that would promote better medical outcomes. This was the CDC’s vision, as laid out with Meaningful Use guidelines.
Are we there yet?
Envision Health Partners along with GLocalMind conducted a survey of physicians (primary care, oncologists, cardiologists and neurologists) in the United States to explore some of these issues. This article explores US physician perspectives on technology and whether it has helped them spend more time with their patients.
The results, revealed in August 2018, suggest that while we have made progress in the right direction, we have “miles to go before we sleep” – and there is convergence around this perception. For example (Source 1), Stanford Medicine worked with The Harris Poll to conduct a comprehensive national survey of primary-care physicians (PCPs) about EHRs. That study, published in June 2018 shows that, “on average, physicians spend a majority of their patient care time (62%) interacting with EHRs”. This intensive relationship with EHRs takes a toll: seven out of ten physicians said that EHRs “greatly contribute to physician burnout” and nearly half believe EHRs detract from their clinical effectiveness”.
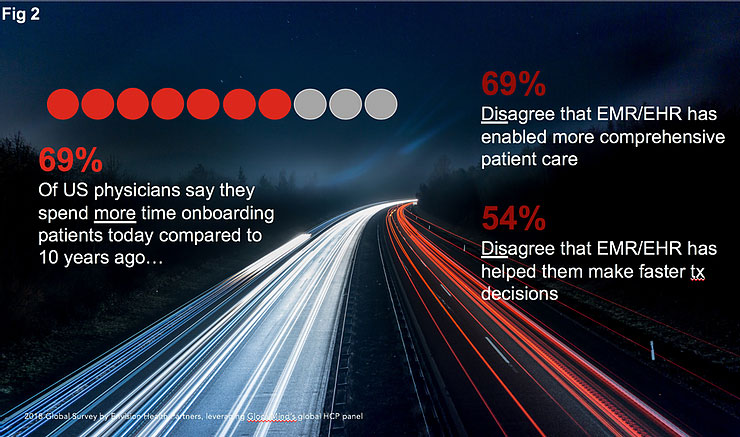
Our own study showed, across all specialists we surveyed, that a majority still feel that they spend more time on-boarding patients compared to 10 years ago and that EMR/EHR systems do not fulfil the promise of being able to make faster or more comprehensive treatment decisions.
According to a former senior outcomes executive at a leading EMR company, who oversaw successful installations of large EMR systems at various kinds of physician practices, small and large, the initial rush to install systems was great. The demand was high and yet there was little guidance on core design elements or a view to ensure interoperability between systems. Indeed it was quite the opposite, with EMR vendors seeking to carve their own niche in the market with full service solutions. Over the past decade, there has been significant consolidation in the space, though the initial gaps created around interoperability remain.
What’s the hold up?
There are myriad articles that have focused on what might be stymying the vision. Many if not most, boil down to assessing that these systems have enabled more efficient coding and billing at the cost of patient care…..and that we are forcing clerical burdens on a highly skilled and trained physicians. A staggering 85% of US physicians in our study say they are spending more time on administrative tasks than a decade ago.
Furthermore, comparing to the past decade, here is what US physicians are saying about their ability to focus more on patient care today.

Fortunately, our study offers a ray of hope.
Self-styled techy-savvy practices, defined as having “seamless digital communication between HCPs and patients” say that they have indeed experienced some of the advertised benefits of EHR/EMRs. These practices, tend to be within or affiliated with hospital systems, so it is likely they’ve made significant investments to ensure interoperability. Still, it makes us want to dig deeper into such practices to see how they have managed to realize the promised benefits and how we can help to enable these benefits more broadly. How have they leveraged the physicians’ data entry efforts to drive faster and better care to patients?
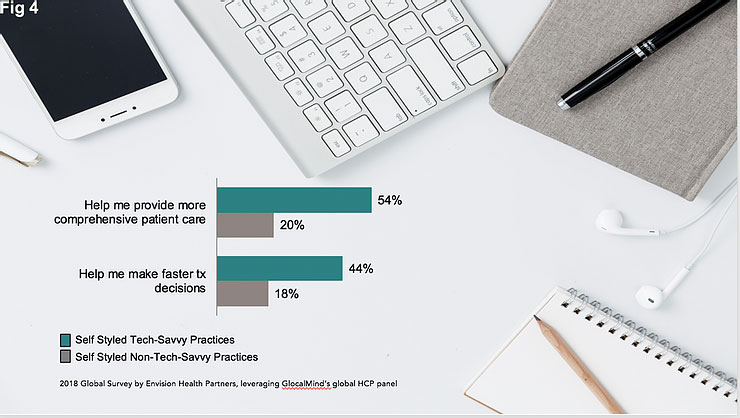
Dr Sakore, Director of Meaninful Use at Northwell Health, one of the largest healthcare networks in the country, validated the finding that larger systems like theirs have definitely benefited from the investments to make EMR systems within the network communicate with each other. Today however, the levels of investment involved to ensure interoperability suggest that organizational reach and scale will matter – ROI is best when patient data is aggregated for population health management purposes. For the benefits to scale more broadly, the costs of such systems integration efforts will have to dramatically drop.
Where are we headed?
There are so many exciting predictions for the future of healthcare (Source 2). At least two of them can directly accelerate our understanding of patients in various ways, and can power the evidence captured in EHR/EMR systems today.
The increasing focus on real-world evidence with healthcare and life science companies dedicating resources to support accessing, sharing and analyzing of such data for use across their organizations.
Passive biometrics, digital health tracking tools that will allow patients to create, store and share their own data with healthcare systems, giving them a greater voice in treatment decisions being made for them.

The Reality:
As always, the challenge will be integration, assuming health policy and regulation will pave the way rather than present more hurdles. Will it be the likes of Apple Health, Google and others, who will take on the data integration challenge and push us forward? Will they be able to navigate the significant hurdles of data privacy and security? Will such innovation finally put the patient rightly at the center of their own data and decisions driven by such data?
What are your thoughts on these findings? For a fuller review of the market research survey results, email us.
Logically, it would seem that involving patients earlier is better, however therapy area nuances impact which stakeholders should get involved early in the development process and where patients can best contribute. It takes vision, leadership, empathy ….and a good understanding of the patient and other stakeholders, to consider various perspectives in early stage planning.
At Envision Health Partners, we are passionate about helping you get insights from the right set of stakeholders, including the patient, to maximize clinical and commercial success. Get in touch to see how we can help.
++++++++++++++++++++++++++++++++++++++++++++++++++++++++++
For a fuller review of the market research survey results, email us.
Authors:
Madhunika Raghavan, Managing Partner, Envision Health Partners and,
Christine LaFiura, Managing Partner, Envision Health Partners
Data Powered By: GLocal Mind’s proprietary panel of healthcare practitioners

@Envision Health Partners:
Headquartered in US, Envision Health Partners is a full service global market research consultancy. Focused on early stage pipelines, Envision Health Partners brings HCP and patient insights to impact clinical trial design and influence market making strategies.
Contact: mraghavan@envisionhealthllc.com;
Website: envisionhealthpartnersllc.com

@GLocal Mind:
GLocal Mind is a global healthcare data collection company. Leveraging their high-quality physician and allied healthcare professionals panel, and a good understanding of local markets, they work collaboratively to support qualitative and quantitative market research needs. 900,000+ panelists are carefully recruited using double opt-in, permission based techniques thus providing a high quality and diverse global panel that includes physicians across specialties, KOLs, Payers, Nurses, Dentists, Veterinarians, Ophthalmologists, Opticians and Pharmacists.
Contact: Vrinda.d@glocalmind.com;
Website: www.glocalmind.com
Sourcing:
- Fortune.com article By LLOYD MINOR June 5, 2018. Lloyd B. Minor is the Dean of the Stanford University School of Medicine.
- www.idc.com
- https://www.rasmussen.edu/degrees/health-sciences/blog/healthcare-technology-trends/
- https://www.healthitoutcomes.com/doc/technology-trends-to-shape-healthcare-in-0001
- https://www.healthdatamanagement.com/list/top-10-predictions-for-healthcare-it-in-2018


