COVID-19 & Silver Linings for the US Healthcare System

COVID-19 will change us. It will change our culture, how we interact with one another, what we prioritize. It will change how we work, how we play, how we travel and how we parent. And it will undoubtedly change the face of the US Healthcare System.
Of course, no one can be fully prepared for an emergency and even the US, despite the world’s highest score on the Global Health Security Index(1) fell short in terms of a speedy response in many areas. That said, we wanted to find a way start a conversation about the kinds of positive changes coming as a result of the pandemic, rather than focus on the shortcomings of our system, and of our response.
Who better to enlist to help create a vision of the future, but those on the very front line of this! Envision Health Partners and GLocalMind teamed up to speak with 8 HCPs (Primary Care, Intensivists, Pulmonary Specialist and Emergency Medicine) treating patients with COVID-19 in the US. We are so grateful to each of them – for their service and their enthusiasm to share their thoughts on the long-term impact of this pandemic on our health care system.
So first, we have to acknowledge how our health care practitioners on the front line candidly felt, about dealing with the pandemic. They used these words to describe their feelings.
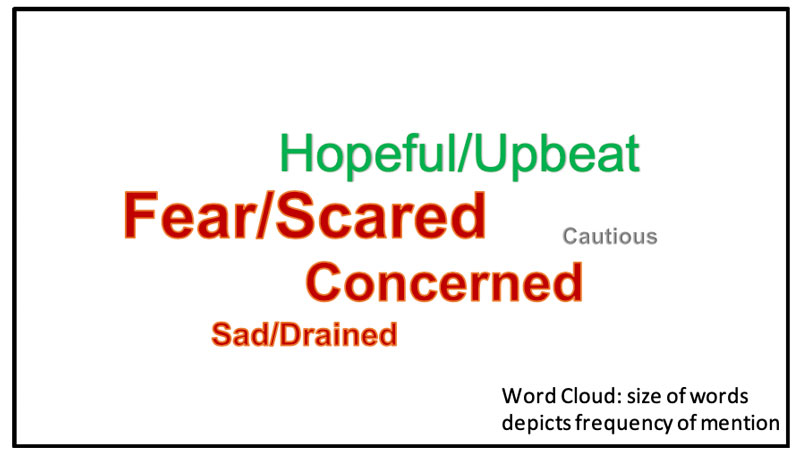
For all, life has turned topsy-turvy since the pandemic – longer hours, great and deep sadness for the lives lost and a primal fear for their own safety and the safety of their families and loved ones.
Fear was a primary emotion – Several of the doctors feared for their patients, and for themselves during this time – the fear of becoming ill, making own family sick or infecting other patients. There was also fear of running out of protective gear, especially at the peak of the crisis.
Physicians also shared the uncertainty they felt around the pandemic – survival rates and if patients were receiving the best care possible; there was also uncertainty about a second wave and if we as a nation, were prepared to handle.
And several were hopeful and upbeat! And every one of them appreciated the opportunity to brainstorm a better tomorrow, and a stronger US healthcare system.
As the world seeks to make sense of the challenge upon us, comparisons to the 1918 Flu pandemic keep arising. These comparisons are usually with regard to the sweeping death rates and the consequences of re-opening too soon, but the 1918 Flu pandemic also changed the face of public health. It led to the origination of national disease reporting systems, revamped health ministries, international coordination and a lessening of a eugenic approach to treatment(2) – many of the underlying principles that we take for granted today. In the spirit of not letting a good crisis be wasted, there will be innovation and transformation from the COVID-19 pandemic.
So, how do we believe the US Health System will change as a result of the COVID-19 pandemic?
Here are some interesting hypotheses we have uncovered in our conversations:
Credible and timely sources of information are sorely lacking; who will step up to this challenge?
- Government health agencies (WHO, CDC, NIH) must self-examine why information from them is often not considered sufficient, timely or credible?
Health care delivery systems will transform in many ways; the most notable of these is in the area of telemedicine. With COVID-19, globally we found ourselves essentially locked into our homes, unable to access our normal channels of care, offering a giant test case for creative uses of telemedicine – and we witnessed a technology driven transformation – telemedicine is now the boon rather than the bane for patients, health care professionals and insurance companies alike.
- The pandemic has allowed us even more sharply to see that telemedicine can have benefit in not only chronic care but in also acute situations (monitoring patients to determine if hospitalization is needed, video consultations for ICU patients, monitoring high risk patients in the ICU, monitoring patients after hospital discharge, etc.).
- Payers have quickly pivoted to cover telemedicine-based services to be seen as doing their part to support pandemic efforts.
Physician licensing practices are expected to come under scrutiny – we have a tangled web of federal and state regulations that control physician licensing. Although federal standards govern medical training and testing, each state has its own licensing board, and doctors must procure a license for every state in which they practice medicine (with some limited exceptions for physicians from bordering states, for consultations, and during emergencies). This bifurcated system makes it difficult for physicians to care for patients in other states, and in particular impedes the practice of telemedicine. The status quo creates excessive administrative burdens and likely contributes to worse health outcomes, higher costs, and reduced access to health care(3).
- With the declaration of emergency, this has come under scrutiny as an additional layer of complexity and bureaucracy that must come undone so that precious talent and resources can be more easily deployed.
- The actively licensed physician to population ratio has increased over time from 277 physicians per 100,000 population in 2010 to 295 physicians per 100,000 population in 2016, but the state by state variations are wide(4) – the combination of telemedicine and the easing of licensing requirements could be powerful to more effective coverage of the population.
There will be a push for preventive care and services and honest conversations on health.
- With COVID-19 having deadlier consequences for patients with underlying co-morbid conditions, physicians say they will be more aggressive with counseling patients to take better care of themselves.
- Physicians feel this pandemic will place greater emphasis and vigilance on hygiene – of public places and health care facilities including physician offices – and we now tacitly have permission to “say something when you see something” not quite up to snuff in these areas.
- Physicians will be more candid with health and wellness advice, especially for patients who are perceived to persist with unhealthy habits and routines.
The pandemic has also laid bare the unequal access of people to our health care system, and will vigorously revive the argument of whether healthcare is a right and must be made available to all or if healthcare is a privilege for the ones who can afford it.
- At no other time in our lifetime, has a single health problem affected every citizen (and non-citizens) in one way or another, and it has brought the healthcare debate into sharper focus.
There are significant changes in play here – policy, infrastructure and regulatory. There are also significant health care delivery model innovations. These in particular, present health care companies (pharma, biotech, devices, diagnostics, etc.) new opportunities to support patients and providers.
How can we re-imagine health care delivery? Follow us on this blog series where we share some ideas and welcome yours, for a robust discussion of how we can together learn from COVID-19 and use our collective wisdom to transform US healthcare delivery to the benefit of patients and providers.
++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++++
Sources:
2- https://www.smithsonianmag.com/history/how-1918-flu-pandemic-revolutionized-public-health-180965025/
3- https://www.healthaffairs.org/do/10.1377/hblog20140218.036973/full/
4- https://www.fsmb.org/siteassets/advocacy/publications/2016census.pdf

@Envision Health Partners: Headquartered in US, Envision Health Partners is a full-service global market research consultancy. Focused on early stage pipelines, Envision Health Partners brings HCP and patient insights to impact clinical trial design and influence market making strategies.
@GLocal Mind: Headquartered in the US, GLocal Mind is a provider of global healthcare data collection services. Leveraging our global panel of physician and allied healthcare professionals panel and a good understanding of local markets, we work collaboratively to support our market research client’s qualitative and quantitative research needs. Our panelists are carefully recruited using double opt-in, verification techniques, providing our clients a robust and diverse global panel. Our panel includes physicians across specialties, KOLs, Nurses, Dentists, Veterinarians, Ophthalmologists, Opticians, Pharmacists, Payors. GLocal Mind’s quantitative services range across programming, hosting & translation, data collection, data processing, custom charting and incentive handling across 50+ countries including key markets in Americas, EU5, Nordics, APAC and Middle East. Our Qualitative services include recruitment, scheduling, moderation, interviewing, translation, report writing and content analysis.

